March 2024
·
16 Reads
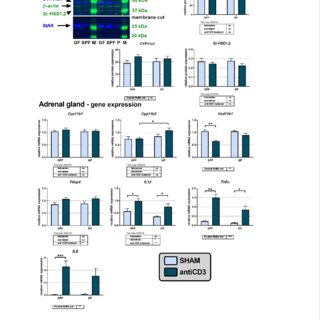
Butyrate, a metabolite produced by gut bacteria, has demonstrated beneficial effects in the colon and has been used to treat inflammatory bowel diseases. However, the mechanism by which butyrate operates remains incompletely understood. Given that oral butyrate can exert either a direct impact on the gut mucosa or an indirect influence through its interaction with the gut microbiome, this study aimed to investigate three key aspects: (1) whether oral intake of butyrate modulates the expression of genes encoding short-chain fatty acid (SCFA) transporters (Slc16a1, Slc16a3, Slc16a4, Slc5a8, Abcg2) and receptors (Hcar2, Ffar2, Ffar3, Olfr78, Olfr558) in the colon, (2) the potential involvement of gut microbiota in this modulation, and (3) the impact of oral butyrate on the expression of colonic SCFA transporters and receptors during colonic inflammation. Specific pathogen-free (SPF) and germ-free (GF) mice with or without DSS-induced inflammation were provided with either water or a 0.5% sodium butyrate solution. The findings revealed that butyrate decreased the expression of Slc16a1, Slc5a8, and Hcar2 in SPF but not in GF mice, while it increased the expression of Slc16a3 in GF and the efflux pump Abcg2 in both GF and SPF animals. Moreover, the presence of microbiota was associated with the upregulation of Hcar2, Ffar2, and Ffar3 expression and the downregulation of Slc16a3. Interestingly, the challenge with DSS did not alter the expression of SCFA transporters, regardless of the presence or absence of microbiota, and the effect of butyrate on the transporter expression in SPF mice remained unaffected by DSS. The expression of SCFA receptors was only partially affected by DSS. Our results indicate that (1) consuming a relatively low concentration of butyrate can influence the expression of colonic SCFA transporters and receptors, with their expression being modulated by the gut microbiota, (2) the effect of butyrate does not appear to result from direct substrate-induced regulation but rather reflects an indirect effect associated with the gut microbiome, and (3) acute colon inflammation does not lead to significant changes in the transcriptional regulation of most SCFA transporters and receptors, with the effect of butyrate in the inflamed colon remaining intact.